Finding Strength At a Time of Crisis
Health system leaders collaborating, learning, sharing—and helping each other navigate the response to COVID-19.
The COVID-19 pandemic has put nurses and other professionals on the frontlines of the biggest healthcare challenge of the past century. Showing passion, resilience, creativity and compassion, these workers are not just rising to the occasion—they are also raising each other up by collaborating, sharing their experiences and learning from each other. Over the course of the past month, more than 90 individuals, representing 40 healthcare systems from across the country, have met weekly to share the lessons they are learning, the successes they are having and the best practices they are implementing to protect patients and caregivers. TeleTracking’s clinical team members, many of whom are featured in this issue of PFQ, also joined the calls offering additional insights and advice.
This story can be found in the 2020 Spring Issue of TeleTracking's Patient Flow Quarterly Magazine. Download the full issue.
The health systems who are part of this conversation include:
Beth Israel Deaconess Medical Center in Boston, MA
Carilion Clinic in Roanoke, VA
Huntington Hospital part of Northwell Health in New York, NY
Kettering Health Network in Dayton, OH
Methodist Healthcare in San Antonio, TX
University Medical Center of El Paso in El Paso, TX
SSM Health in St. Louis, MO
Freeman Health System in Joplin, MO
Avera Health in Sioux Falls, SD
These are some of the nation’s foremost experts in disaster and incident response, having managed through mass shootings, tornados and hurricanes—and who are now bringing their expertise to the COVID-19 pandemic. They are also leveraging their Command Centers to track vital resources such as ventilators on a system-wide basis, add and manage new beds at alternative care sites, and provide visibility to suspected and confirmed COVID-19 cases in real-time for all stakeholders. Below is a sampling of COVID-19 recommendations and best practices shared to date.
WHAT WE ARE LEARNING TOGETHER
 Incident Command Center/Health System Command Center COVID-19 Best Practices
Incident Command Center/Health System Command Center COVID-19 Best Practices
Kettering Health Network’s Incident Command Center, located adjacent to its Network Operations Command Center, was established in early March and includes members from nearly every operation across the network—including marketing and communications; nurses and physicians; data analysts; logistics, operations, lab services and infection control staff; police departments, etc. As Kettering ramped up for COVID-19, the ability to get information in real-time was essential, and the TeleTracking COVID-19 dashboard has made it possible to look at metrics hour by hour. The team at Kettering knew the processes and data that was necessary to effectively manage a large-scale health crisis like the COVID-19 pandemic after dealing with a major tornado and a mass shooting within a few months last summer.
The Incident Command Center at Beth Israel Deaconess Medical Center is sharing information about capacity at each hospital—including community hospitals—as well as available ventilators. Senior staff members meet morning and afternoon to share critical capacity information.
The Carilion Clinic Transfer and Communications Center (CTaC) makes it possible to quickly and easily share and communicate information across the system. For example, the CTaC can identify negative pressure rooms, in real time, at an enterprise level and prioritize patients that can be moved in order to open space for incoming patients. The CTaC is also responsible for indicating persons under investigation (PUI) for COVID-19 and when a bed is needed they can quickly assess the location of available beds across the system in TeleTracking and start the patient transfer/admission.
 Preparing for the Surge
Preparing for the Surge
Methodist Healthcare in San Antonio started its preparations in early February after receiving notification from the Southwest Texas Regional Advisory Council (STRAC) that American citizens returning from Wuhan, China would be sent to the Joint Base San Antonio-Lackland military base. Citizens who showed signs and symptoms for COVID-19 would then be transported to Methodist Hospital for care. Approximately 100 American citizens were housed on the base. Three citizens were transported to Methodist Hospital, with one testing positive for COVID-19. This patient remained at the hospital for approximately one week. Joint Base San Antonio was also where 300 passengers from the Diamond Princess cruise ship were evacuated upon arriving back in the United States. One patient tested positive for COVID-19 and was also cared for at Methodist. Methodist continued to prepare for what the pandemic would look like, with things being slow, at first. However, that changed around the time of spring break, with an increase of cases that appeared to be travel-related with people returning from New York, New Orleans and Colorado. All Methodist Healthcare facilities implemented surge plans and developed COVID-19 cohorting units. To expand capacity within Methodist Healthcare, an ambulatory surgery center was transformed into a COVID-19 facility within 48 hours.
Administrators from UMC El Paso started meeting in mid-February, and by March, it was all hands-on deck. UMC El Paso has done many disaster preparation drills, and having responded to a mass shooting incident last August, the team knew they were ready for just about anything. Organizing teams and organizing information was very important early on. Custom views in TeleTracking were created for leadership to track, in real-time, the volume of patients and those testing positive or negative for COVID-19, and read-only views are being shared with pharmacy, respiratory and food service for increased visibility—and to maintain staff safety. Engineering also expanded the number of negative pressure rooms by placing exhaust fans in windows. El Paso, TX is seeing on average 40-50 positive cases every day, for a total of more than 400 cases to date, and the spike was projected for early May.
Northwell Health’s Incident Command Center opened in early March and has been staffed 24 hours a day for the last 45 days. The critical role that TeleTracking plays in managing patient logistics across the system was evident when Governor Cuomo instructed hospitals in New York to increase capacity by 50 percent. Northwell Health has added 1,000 additional surge beds since the pandemic started. For tracking purposes, Northwell is using TeleTracking to indicate the location of the newly added beds. Huntington Hospital, for example, converted PACUs, catherization labs and vacant emergency room spaces into additional ICU beds since elective surgeries have been canceled or delayed. And nurses working in other units stretched their skills to heroic levels treating critical care, ventilated patients. The team is also load-balancing patient care across the Northwell system, helping out their sister hospitals.
SSM Health was charged with increasing capacity in two phases—in the first phase 140% and in the second phase 180%. This rapid level of expansion meant that alternative care sites [ACS]—such as the pediatric hospital and nearby hotels—had to be quickly operationalized. For example, hotels are set up to accommodate patients who are ready to be discharged from an acute care facility, but still need to remain in quarantine or isolation because they have a loved one at home that is elderly or immunocompromised, or their home is an assisted living facility that is not accepting COVID-19 patients. SSM Health is the central point of contact for these placements—they obtain the patient information and the discharging doctor’s information, then connect the discharging doctor to the ACS doctor and facilitate the acceptance. Then they obtain the patient room and arrange transportation.
 Managing Visitors
Managing Visitors
Freeman Health System started limiting visitors in mid-March to one person, per patient, per day and needed to be able to track them. The team decided to use the miscellaneous field in the patient placement details section in TeleTracking to enter the date, visitor name, and time that the visitor arrived and departed. A patient audit report could then easily export the visitor information for sharing and tracking purposes. Even with needing to train 250 employees and volunteers who were processing the visitors, the program was brought online in just a few days.
 TeleHealth
TeleHealth
Avera Health serves about a million people, but across a very large swath of land—communities in South Dakota, Nebraska, Iowa, Minnesota, and North Dakota. They do this through six regional healthcare centers and 35 community access hospitals—but in many ways it is frontier medicine. Avera eCare provides e-emergency, e-ICU, e-pharmacy, and e-longterm care— helping to bridge the gap for rural healthcare partners to retain patients within their own facilities. They have also invested a great deal of work into maximizing their command center to load-balance across their regional hospitals through the support of the eCare network—connecting them to cardiologists, pulmonologists and other critical care doctors. The team is also using iPads on COVID-19 units of the hospital(s) so that physicians can do remote rounding to reduce contact and as a way of conserving PPE.
 Identifying COVID-19 Patients
Identifying COVID-19 Patients
Of the systems that have shared stories to date, all are using COVID-19 patient attribute icons in TeleTracking to indicate patients that are under investigation versus confirmed for COVID-19. These icons are displayed on electronic whiteboards on hospital units so that caregivers can quickly see patient status. The hospitals are also tracking positive cases of COVID-19 through an isolation report in TeleTracking to ensure caregivers take precaution and have appropriate PPE, and to indicate if caregivers have been exposed to an infected patient. Many of the hospitals are also cohorting COVID-19 patients.
 Reports & Dashboards
Reports & Dashboards
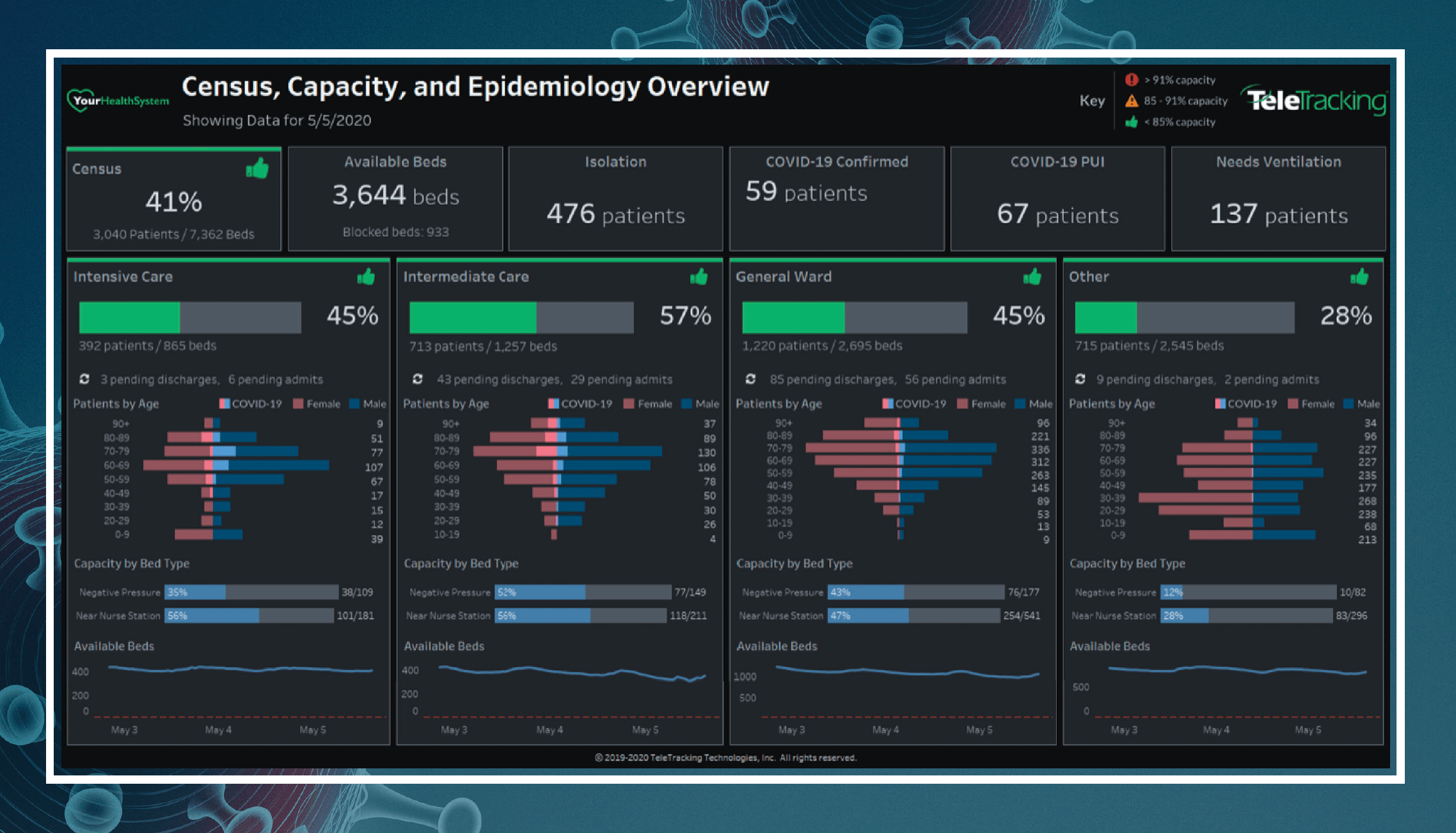
TeleTracking released an enterprise COVID-19 capacity and census dashboard to its SynapseIQ Enterprise customers on April 1, 2020 to equip health systems with the critical information needed to prepare for and respond to the COVID-19 patient surge. The dashboard provides real-time information related to patient census, bed availability, confirmed and possible COVID-19 patients, patients in need of ventilation, capacity of specialized treatment areas such as negative pressure and ICU rooms and patients by age. The dashboard is also available to hospitals currently using TeleTracking Capacity Management Suite™ version 3.4 or greater.
Methodist Healthcare developed and deployed a COVID-19/PUI COVID-19 count dashboard that is displayed in the Incident Command Center and Patient Placement Center with real-time updates as patients progress through the testing process. Methodist Healthcare also created a census epidemiology dashboard in TeleTracking SynapseIQ® Enterprise, which is updated in real-time and is also displayed in the Incident Command Center.
Carilion Clinic is using the TeleTracking COVID-19 dashboard to show the number of confi rmed COVID-19 patients, those that have been ruled out, the location of each patient, in addition to other critical metrics.
 Sticking Together
Sticking Together
Kettering Health Network and neighboring, competing health systems are working together to share information and stay connected. Methodist Healthcare and UMC El Paso are already thinking through different scenarios and lessons learned to improve processes related to disaster preparedness and infectious diseases. Carilion Clinic has expanded their CTaC to include a number of large monitors so that at a glance all are aware of the current status. Huntington Hospital is load-balancing patient volume, forecasting what the needs are of the day within the hospital, and using the projected census to determine patient volumes each day.
 The common thread—a centralized approach to care helps maximize valuable resources, provides vital visibility into bed capacity, improves care and safety for patients and protects the health of caregivers.
The common thread—a centralized approach to care helps maximize valuable resources, provides vital visibility into bed capacity, improves care and safety for patients and protects the health of caregivers.
We're glad you're enjoying our resources! Please tell us more about you to access our full library.
This will allow us to personalize your experience on TeleTracking.com. Of course, we will never sell your information and you can opt-out at any time. Need help now? Contact a Patient Flow expert.
Leaving the website
You're about to leave this website, to one of our affiliates or another information source.